
Why Airway Health Matters
A clear and open airway is essential for proper breathing, especially during sleep. Children with restricted airways often struggle with mouth breathing, snoring, or even obstructive sleep apnea (OSA).
Poor Airway = Poor Sleep
When children don’t get quality sleep, it can affect:
· Brain development and behavior
· Growth hormone production
· Mood, attention, and school performance
· Immune function
Mental Health Impacts
Children with airway disorders often experience an emotional element that can be misdiagnosed as ADHD or, worse, disregarded. Daily strain from living with a breathing disorder can wear on a child’s mental capacity. No child should be depressed from sleep issues or be at risk of hypoxic

Signs and Symptoms of a Sleep-Disordered Child
- Snoring or heavy breathing during sleep
- Restless sleep or frequent waking
- Night terrors and bedwetting beyond early childhood
- Daytime fatigue or hyperactivity
- Persistent Mouth breathing
- High V-shaped palate
- Receding lower jaw; retrusive chin
- Scalloping on tongue edges
- Severe malocclusion
- Dark circles under the eyes ("allergic black eyes")
- Constant nasal congestion and/or runny nose
- Forward head and neck posture
- Frequent earaches and tonsilitis
- Poor weight and failure to thrive
These symptoms could be clues that your child’s airway is compromised.
What To Look For During Sleep
Is the child quiet? Sleeping soundly, mouth closed, no breathing sounds, and no teeth grinding (Bruxism)
Is the child dry? Lips together, no open-mouth or drool on the pillow, no night sweats
Is the child still? Sleeping comfortably with little movement, and no restless tossing and turning or sleep walking
What is Proper Tongue Posture?
Proper tongue posture means the entire tongue rests gently against the roof of the mouth (the palate)
when you're not talking or eating.
It should be:
· Lips closed
· Tongue sealed to the palate, especially the middle and back
· Breathing through the nose
How Tongue Posture Affects the Airway & Breathing
- Supports Nasal Breathing
· A tongue that rests on the palate naturally encourages nasal breathing by helping keep the
mouth closed.
· Nasal breathing is healthier than mouth breathing—it warms, filters, and humidifies air, and
supports nitric oxide production (which helps oxygen delivery). - Shapes the Upper Jaw and Palate
· The tongue is a natural "expander" of the upper jaw.
· When it rests on the palate, it stimulates proper growth of the upper jaw (maxilla) outward and
forward.
· A well-developed maxilla = wider airway space behind the nose and throat. - Prevents Narrow, High Palates
· Without tongue pressure, the palate may grow high and narrow, which restricts the nasal
airway and contributes to mouth breathing.
· Narrow palates are often linked with crowded teeth and underdeveloped midfaces. - Improves Tongue Position During Sleep
· A low tongue posture (resting in the bottom of the mouth) falls backward during sleep, which
can block the throat and restrict airflow, increasing the risk of snoring or obstructive sleep
apnea.
· A well-positioned tongue stays forward and up, keeping the airway more open.
Long-Term Benefits of Good Tongue Posture
· Better oxygen flow during the day and night
· Improved facial development (especially jawline and cheekbones)
· Reduced risk of sleep-disordered breathing
· Healthier bite alignment and less need for major orthodontic or surgical correction later
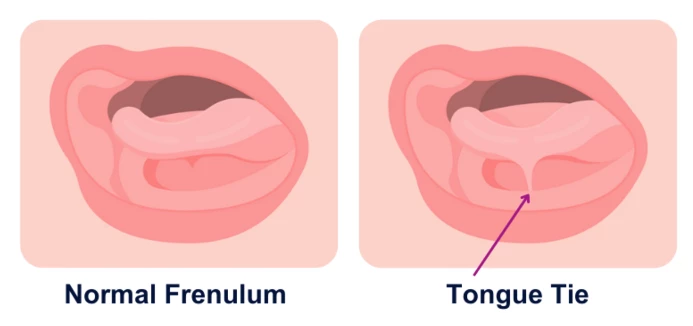
Tongue Tie
Tongue Tie = Poor Tongue Posture
When the tongue can’t move freely, it often:
-
Sits low in the mouth
-
Can’t reach the roof of the mouth
-
Can’t function properly during swallowing, speaking, or at rest
What Can Help?
Tongue Tie Evaluation:
A trained provider (myofunctional therapist) can assess if your child has a functionally restrictive tongue tie.
Release (Frenectomy or Frenuloplasty): If needed, a gentle procedure can free the tongue, allowing for better posture and movement.
Myofunctional Therapy: Exercises to help retrain the tongue and oral muscles—often combined with orthodontics like maxillary expansion for full benefit.
Orthodontic Support: Maxillary expansion can improve space in the palate so the tongue has room to rest where it belongs.
Note: Poor tongue posture is not always due to a tongue tie. Poor tongue posture can be simply poor tongue tone, strength, and stretch. A myofunctional therapist would start working with tongue exercises to first see if the tongue can be positioned properly in the roof of the mouth. If myofunctional therapy alone does not help, a tongue tie release may be needed. It is VERY important to take these steps in a certain order to prevent the tongue from tying back down, sometimes even more severe than the initial tongue tie.
When Bigger Isn’t Better: Enlarged Tonsils & Adenoids and Their Impact on Airway Health
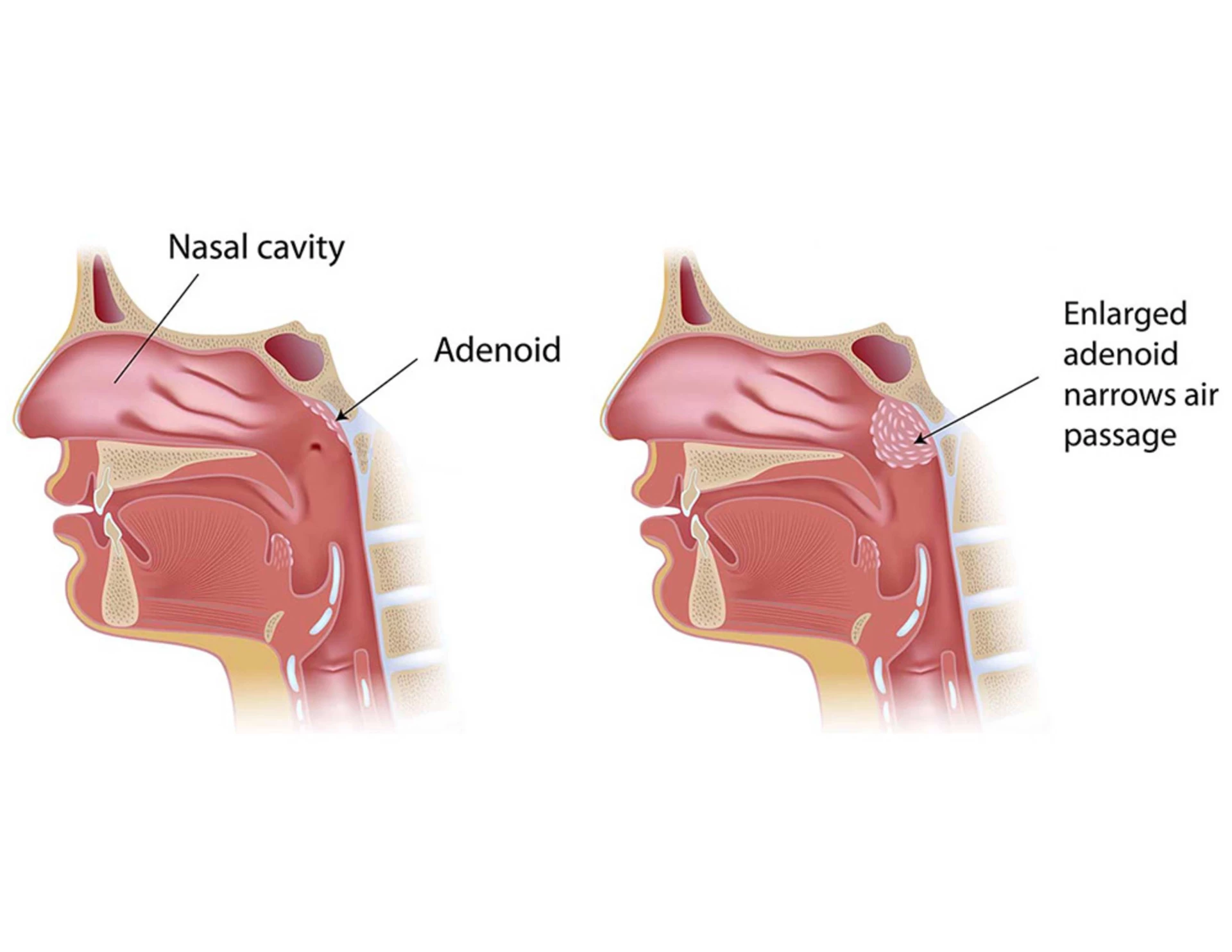
What Are Tonsils and Adenoids?
-
Tonsils are two lymph nodes located at the back of the throat.
-
Adenoids are a patch of lymphatic tissue located higher up, behind the nose, where you can’t see them.
They help fight infections—but in many kids, they become chronically enlarged, especially due to allergies, frequent illnesses, and even due to a narrow palate and mouth breathing.
How Do Enlarged Tonsils & Adenoids Affect Breathing?
Airway Obstruction
-
Large tonsils can block the back of the throat, and enlarged adenoids can block the nasal passages, making it harder to breathe—especially during sleep.
Mouth Breathing
-
If the nose is blocked by adenoids, kids may breathe through the mouth by default, which:
-
Dries the mouth and airway
-
Contributes to poor tongue posture
-
Interferes with facial and jaw development (narrow, high vaulted palate)
Interrupted Sleep & Sleep Apnea
-
Blocked airways can cause:
-
Snoring
-
Pauses in breathing (apnea)
-
Restless sleep
-
Nighttime awakenings
This disrupts deep, restorative sleep and may lead to:
Daytime fatigue
Trouble focusing in school
Hyperactivity or behavioral issues
Delayed growth (since growth hormone is released during deep sleep)
What Comes Next?
Sleep Study: In some cases, a simple sleep study (polysomnography) can help confirm sleep apnea or breathing issues.
Surgical Removal (Tonsillectomy & Adenoidectomy): If the tissues are significantly blocking the airway, surgical removal may be recommended—often with dramatic improvements in sleep, breathing, and behavior.Orthodontic Collaboration:
Orthodontic treatments like maxillary expansion can help improve nasal airflow and reduce the impact of enlarged adenoids.
What Can Be Done?
ENT Evaluation: An ear, nose & throat specialist can assess the size of your child’s tonsils and adenoids, especially if sleep-disordered breathing is suspected.
Sleep Study: In some cases, a simple sleep study (polysomnography) can help confirm sleep apnea or breathing issues.
Surgical Removal (Tonsillectomy & Adenoidectomy): If the tissues are significantly blocking the airway, surgical removal may be recommended—often with dramatic improvements in sleep, breathing, and behavior.
Orthodontic Collaboration: Orthodontic treatments like maxillary expansion can help improve nasal airflow and reduce the impact of enlarged adenoids.
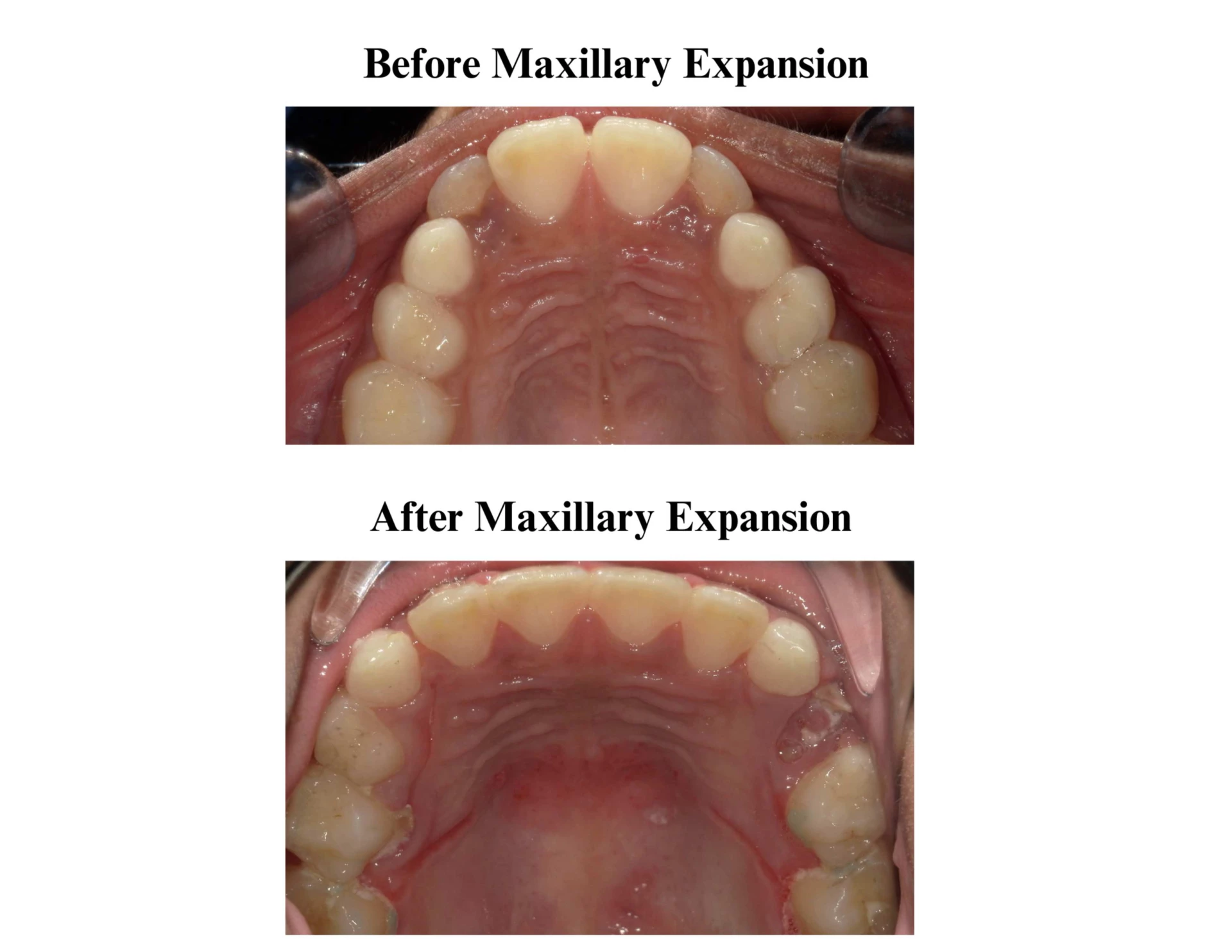
How Orthodontics Can Help
The Role of Maxillary Expansion
Maxillary (palatal) expansion is a gentle orthodontic technique that widens the upper jaw. It can:
-
Increase nasal airway volume
-
Improve breathing through the nose
-
Reduce mouth breathing and snoring
-
Support proper tongue posture by creating more space in the palate (with the help of myofunctional therapy)
-
Help align teeth and jaws for a more functional bite
-
Help reduce size of adenoids or prevent enlargement again after removal
Note: Expansion at the ages of 5-8 can significantly improve the nasal airway. Expansion in the later ages have less of an effect on the nasal airway volume and sometimes more invasive procedures have to be done for optimal results.
Give Your Child the Gift of Breath and Rest
Early Orthodontic Evaluation is Key
The American Association of Orthodontists recommends that children get their first orthodontic check-up by age 7. Why? Because early signs of airway or jaw development issues can be identified and treated more easily at an early age.
Let’s work together to help your child breathe better, sleep deeper, and grow healthier.
Credit: Children’s Airway First Foundation
Hours
Mon-Thu:
7:00am - 4:30pm
You can reach us by phone outside of our regular business hours!
Monday-Friday 8:00 AM - 11:00 PM
Saturday-Sunday 10:00 AM - 6:00 PM